I’ve recently published a new book about low iron stores in runners. Nexus Magazine requested an article and I have submitted this:
Low Ferritin
Is this a Canary in the Coal Mine?
Most people have never heard of low ferritin, let alone appreciate the subtle causes behind it. Yet, there is a fairly high probability that the average civilized person suffers from “low iron stores” to some degree whether officially diagnosed or not.
Low ferritin is merely a medical test marker which identifies the amount of iron in the blood. There are a series of falling Dominos that lead to the condition itself. And then there are other consequences which can follow, if the cause is not recognized and left untreated, symptoms which fall below the threshold of awareness until serious.
It’s like the dying of coral reefs across the oceans. Scientists can identify that they are disappearing, but a person can’t pull up a chair and watch it happen. Low ferritin as a personal event occurs slowly, although it seems to appear overnight.
My first exposure to low ferritin came by accident after I was filming a friend’s track workout. He coaches high school long distance runners with extraordinary results and I wanted to document his work just for fun.
I noticed that one of his female runners was broken-out with a rash of pimples on her neck. Since I had worked with clients as a “detoxification consultant” for over a decade, I recognized her break-out as not-the-standard teen pimples. I mentioned this to the girl, that she may have some digestive issues behind the rash on her neck and that it would be worth looking into. Her reply was that she knew about it and that her mother was a nurse and they had it under control.
I suggested to her coach that I thought this runner had a disorder which was NOT under control. This high school senior was an exceptional runner and was likely to take first in all the girl’s distance track events at the Tennessee state meet, but my friend told me that she was low in “ferritin,” which had proven to be her #1 constraint to her performance.
I correlated the rash on her neck to her low ferritin. This would be “a no-brainer” to some non-medical health experts. As it turned out, she was seeing two different doctors; one for her skin issues and one for her low ferritin, and so neither saw a relationship of one symptom to the other.
A rash of pimples is not generally associated with low ferritin, so this would be an extreme example of one condition as the underlying cause of both problems. In other words, each issue was being treated as its own type of disease, while I viewed them as symptoms or indicators of a shared, but hidden malady.
The mother of this runner phoned me. She explained that the dermatologist had recommended needle injections of a fungal irritant to the rash in order to stimulate an immune response to that area. In the treatment of low ferritin, her daughter was taking high doses of iron. I had to laugh. Both doctors were actually worsening the conditions being treated by the other!
I then proceeded to explain to the nurse-mother what may be going on and alternative ways to approach it. This took over an hour on the phone and the mother said she was rapidly taking notes. I was rather shocked at how little she knew and how little had been explained to them by her daughter’s doctors.
For me, it was a small learning, a novelty, and I actually didn’t give it much thought.
It was only later, when I learned that low ferritin was affecting other kids on the team that I gave it much consideration.
I told my coach-friend that the problem was this, then that, then that, then this, then that. I made some dietary recommendations related to iron assimilation and his feedback was that his team made notable improvements. His high school boys team at Brentwood High went on to take third place in the prestigious Nike Cross Nationals (NXN), the U.S. national championship race held in Portland, Oregon in December, 2013. For the 2014 track season, his team continues to make headlines.
I researched the running media to see how it was addressing the issue of low ferritin affecting many teams. One study found that over half of runners were low in iron. 1 How this is commonly addressed has been: 1) medically testing runners showing low iron symptoms like chronic exhaustion, usually with the ferritin test, 2) increasing dietary iron intake, and 3) supplementing iron in the form of pills or liquids, with mixed results.
My Background
In 2001, I became a professional colon hygienist. What that means is I administer water into a person’s colon and observe what flushes out. What might strike a newcomer to this field is the huge volume of fecal matter which can make its exit. Of interest to me was the fact that every client was fully backed-up in their colon, no matter their demographic, nor their dietary habits.
The classic understanding of constipation is that it correlates to fiber in the diet. I began to research the topic, looking for another cause to chronically backed-up colons as a social/cultural phenomenon. This search proved successful, although it did not trace to the colon, but to the human liver.
The liver conducts more than 1,500 metabolic functions. One of those is called cytochrome P450 pathway. This is the conversion of fat soluble poisons to a water soluble which can be excreted in urine, sweat, and in stool. Lacking the nutritional sources to conduct cytochome P450 pathway, the liver will store oil soluble toxic substances within its own tissue and in fatty tissue throughout the body. 2
I mentioned “falling Dominos” earlier. The sequence here is: 1) the consumption or absorption of oil soluble chemicals by the individual (food additives, farm chemicals, bug repellents, gasoline fumes, plastics, etc.), 2) the storage of those chemicals within the liver itself, 3) and the impairment and exhaustion of the liver to some degree. Modern civilization’s rampant use of oil soluble chemicals across every industry places us on the general map.
What fails next in this sequence is the liver’s ability to produce a substance called bile. This fluid emulsifies dietary fats and is critical to digestion. Little recognized is the concept that the flow of bile can vary depending on the health of the liver. For my purposes, I put two and two together, correlating a high rate of constipation together with a probable high incidence of low bile flow.
A reduction in bile flow means that unemulsified, poorly digested fat in the digestion-process has at least two consequences.
First, fats abnormally coat food-matter, such that digestive enzymes are prevented from fully accessing nutritive components. Less nutrition would be assimilated through the digestive tract, creating more waste, if this were the case.
Secondly, poorly digested fats would bond to any minerals present in the food, likewise preventing mineral assimilation, while increasing mineral content within the stool, thereby hardening the stool into what many refer to as constipation. High fiber content, in this abnormal digestive sequence, would only serve to further bond to undigested fats like straw in adobe bricks.
The next question is whether this internal “dis-order” has been clinically demonstrated by scientific labs. The answer technically is yes. However, the variables are so many, that isolating each variable as causative down the logical sequence is not possible. Therefore, one cannot technically refer to this or that study proving the sequence that man-made oil soluble chemicals in the liver can cause constipation.
However, we can check the math. If human livers were under a generalized toxic assault, then a mineral such as calcium would be prevented from full assimilation, resulting from its bond to excess fats in the small intestine. Most civilized cultures consume calcium in the diet and supplement calcium more than ever as populations in history. Yet, these same populations suffer from bone loss (osteoporosis) to a degree higher than ever historically. In fact, there is an inverse statistical ratio to what logic says it should be: the higher the calcium intake by nation, the higher the level of osteoporosis.
My point is that calcium ingested does not equate to calcium assimilated, and the same with iron pills, if a person’s liver has been repeatedly assaulted and then exhausted.
When it comes to student runners, my suggestion was to begin supplementing an essential fatty acid oil, which the liver utilizes nutritionally to conduct cytochrome P450 pathway. This would facilitate the liver to self-cleanse and to stimulate more bile production, increasing fat emulsification, providing for a more natural digestive process in which minerals can be assimilated.
I make this dietary suggestion for runners, all athletes, sedentary folks, pregnant women, children, pets, you name it.
More to the Story
There is an additional factor affecting liver function. This would be a disease called cirrhosis. Certainly it would be a stretch to suggest that young runners suffer from a full-blown case of liver cirrhosis. But it is at least noteworthy to mention that cirrhosis involves scarring of the bile ducts and that this can occur at an extremely mild level well-below what medical tests would measure.
Excess alcohol consumption is commonly associated with cirrhosis and this would rarely be a factor for high school runners. What can trigger some measure of liver function impairment as scarring bile ducts are antibiotics.
Oxford Journals, the Journal of Antimicrobial Chemotherapy published an article titled, “Hepatic Safety of Antibiotics Used in Primary Care.” (www. ncbi.nlm.nih.gov) The article noted: Antibiotics are considered as a common cause of drug-induced liver injury (DILI). Although the frequency of serious antibiotic-induced hepatotoxicity is low compared with the amounts prescribed each year — it remains a main reason for antibiotic withdrawal after product launch. Antibiotic-induced hepatotoxicity is usually asymptomatic, transient and associated with only mild hepatic impairment. (Bolding is mine.)
In context, we might want to survey the field for the reason behind why young adults are testing low in ferritin on a significantly large percentage scale, within a fairly narrow range of a contemporary population, which are student runners. It is not a far stretch to identify that runners are a random sample of a population and that the general population may suffer from precursors to low iron stores, also, yet not be testing for it. Plus, historically it’s not possible to test runners from previous generations for low iron stores, yet the condition is significant to note today, while less so yesterday.
It would not be unreasonable to ask whether today’s population is more exposed to antibiotics than previous generations and what those sources might be. It is generally noted that antibiotics are used to raise farm animals such as cows, pigs, and chickens in crowded conditions and that these meats are treated with some form of “sanitization product” to prevent bacterial poisoning in the consumer. This is relatively new to human history. Antibiotics are likewise prescribed as a medicine for humans as a common practice and many household products like mouthwashes are antibacterial.
It might be generally stated that society functions today by a broad application of antibiotics as part of the food supply or as a medicine. Therefore, it is possible to imagine that the consistent intake of foods containing an antibiotic could be causing a mild level of side-effects to the human liver, passing below the threshold of awareness, impairing bile production and flow, reducing dietary fat emulsification and the assimilation of minerals, showing-up on medical tests as “low ferritin.” End of story.
However, why stop there? Antibiotics likewise decimate “friendly bacteria” in the small intestine known as acidophilus. These microflora live as a community of trillions of organisms along the intestinal brush border where iron is assimilated. In order for iron to pass into the blood stream, it must first be saturated in an acidic solution, which acid-dophilus excrete as waste from their own metabolism. In a small intestine, which has lost acidophilus populations, iron assimilation would be difficult, at best.
(Diagram of acidophilus in green lining the small intestine, repelling Candida.)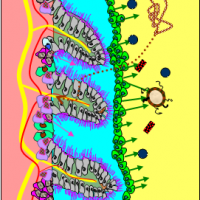
One common side-effect of antibiotics taken as a prescription is Candida yeast overgrowth. Candida yeast likewise reside within the small intestine, but are kept in communal balance by friendly bacteria, whose primary defense is this same acid waste which repels yeasts from the receptor sites where minerals are assimilated. The waste of Candida is acetylaldahyde, highly toxic to the human body, the same chemical which causes an alcohol hangover and which exhausts the adrenal glands. Candida will convert blood sugars into alcohol-waste too, which then pass into the liver.
Thus it is a cycle, a downward spiral of falling events.
The other interesting factor about Candida is its metabolic use of iron. And Candida albicans is immune to antibiotics. Once populations of friendly bacteria are destroyed by antibiotic contact, Candida can freely attach itself to the brush borders of the small intestine. They have the ability to puncture the protective intestinal lining, pass into the blood stream, and translocate to anywhere they have access to iron and sugar. Then Candida directly attack the supply line of iron, which is stolen from a protective protein called transferrin, while on its path to larger iron storage units known as ferritin.
Surprise, surprise!
The iron-poor condition known as anemia is where blood supply is diminished along with iron storage capacity. With most young runners, they have adequate hemoglobin (blood supply) with diminished ferritin. This means that it is possible that something is passing into the blood, which does not interfere with blood production at initial stages, but is able to withdraw iron and lower ferritin-count, or so-to-speak, empty the bank account.
If this was to be Candida, then it entered the blood through puncturing the small intestine, which it could not do with healthy levels of acidophilus present. Thus, this would be a double-whammy to iron, with low assimilation on the front end, and iron-theft by yeast on the back end.
If Candida is behind low iron stores, the liver would produce an antifungal defense against fungal overgrowth called hepcidin. Hepcidin likewise impairs thyroid communication in the liver, causing stomach acid reduction, which impairs vitamin B12 absorption, which further crashes the person suffering from “low ferritin” from gaining meaningful nutrition from their diet, craving sugar as a result.
To check the math, we note that low ferritin and the condition of hypothyroid frequently appear together. Where it ties is at the liver, producing antifungals like hepcidin as a defense against Candida overgrowth, following antibiotics as a prescription or in food as a sterilizing agent.
And there you have it: low ferritin as a ratio result in the balances between harmful yeast and friendly microflora. Plus factoring the liver’s ability to self-cleanse and produce bile. Throwing iron pills down the gullet in the long term fuels the engines to drive even more problems home in the future, including sugar-craving leading to obesity.
The female high school senior who suffered from a pimple-rash on her neck, I believe suffered as a result of her skin attempting to removed fungal acetylaldahyde-waste from her system where she sweat. Of course, I am not a medical professional, so I cannot say for sure. Her mother initially told me that her doctor had her supplementing high doses of iron, which many runners do, which in her case may have accelerated and fueled the metabolic cycle of Candida in her system. Then, that growth of fungal waste quantity inflamed her skin.
Then, skin rashes are frequently treated with antibiotics — with no show of improvement, further supporting future Candida overgrowth and a slow, downward, frustrating spiral.
I suggested that this runner’s nurse-mother consider that her daughter begin consuming fermented foods like miso, kombucha, and plain goat milk yogurt. And to recognize foods in her daughter’s diet such as ground meats, which might contain harmful sterilizing agents, like sausage and hamburger. I suggested that even salads served in chain restaurants are sterilized with high amounts of chlorine as a wash and to try eating more meals at home made from organic ingredients.
The mother asked me about white meat chicken breast, to which I replied, “Research the factory farming of chickens and antibiotic use by those farmers and processors.”
This runner may have had an exceptional season with or without my recommendations, but she did finish her track season with three first place finishes in long distance events at the girl’s state track meet in 2013. It’s called “a triple crown.”
I made these same dietary recommendations to the Brentwood High cross country and track team runners, plus essential fatty acid oils, and for whatever the reason, low ferritin issues resolved themselves during the 2013/14 seasons.
Here’s the reason why. Low ferritin, low iron, and low energy are not individual-specific. These are “cultural issues” affecting civilized populations who are consuming similar foods and suffering from the same illness precursors by varying degree.
Therefore, the best treatment for low iron stores is prevention. And one cannot implement prevention without awareness. And who understands that all this internal mumbo jumbo is real, if not a colon hygienist observing people’s poop?
In history, fermented foods rich in prebiotics and probiotics were the norm for robust peoples, not the exception. Thus, in the case of low ferritin, I suggest that the best path forward will be — backwards.
Link to Low Ferritin: http://www.smashwords.com/books/view/434546
Free access code: XA35J Hit “buy” button, fill in short info request, then input free code. Code expires May 15.
Footnotes:
1 Hunding, Jordal, and Puley, Runner’s Anemia and Iron Deficiency, Journal of Internal Medicine, April 24, 2009.
2 Lipski, Leaky Gut Syndrome, Keats Publishing, 1998.
